Organized by the Governments of Côte d’Ivoire and France, the World Health Organization, the Global Fund to fight AIDS, Tuberculosis and Malaria, and the French civil society platform on drug policy
Camille Spire, French Civil Society Platform on Drug Policy. I am here on behalf of the French NGO platform on drug policy. I thank the Minister of Cote d’Ivoire and UNODC for hosting us today. Why are we here today? A few months before the next Replenishment conference of the Global Fund to take place in France in October, we wanted to highlight the global fund’s role in scaling up harm reduction. The UNGASS OD put health and human rights as pillars of drug policy. It is therefore necessary to further harm reduction in drug policy. This is also highlighted in the 2030 Agenda for Sustainable Development. This event highlights the actions of the global fund through specific examples such as Ivory Coast. We have the pleasure to welcome a broad panel of governments, institutional speakers and civil society speakers.
Dr Aouélé Eugène Aka, Minister of Public Health and Hygiene, Ivory Coast. Thank you very much. It is a great honor to preside together with France, the French civil society platform on drug policy and the support of the WHO and Global Fund, to be present at this side event and discuss the objectives set up by the Global Fund. It is an honor to have been invited and our President has asked me to convey his best greetings.
The fight against AIDS, TB and malaria is key and we are happy to be here today. The health issue is a key objective for international policies. This is also amongst the objectives set out in the 2030 Agenda for Sustainable Development, including deaths among children below 5 years old and the fight against AIDS.
Since the Global Fund was established in 2010, thousands of lives have been saved. We have stopped the spread of HIV and reduced the numbers of deaths. We have launched programmes to treat everyone and we have introduced special training programmes for midwives. Treatment is one of the essential elements we can do in this fight against this terrible disease. We also think of co-financing of our programmes in the fight against AIDS. We have spread good practices and research.
We have seen a reduction in the mortality rate. This allowed for optimal healthcare for the whole population. We have also improved the centres for the diagnosis and treatment of HIV/AIDS.
In the fight against HIV and HCV, we have made a lot of efforts to test everybody. HIV prevalence among pregnant women has also reduced, to 2.5% in 2017. In terms of reductions in deaths from HIV, we also experienced a reduction which has been accelerated: in 2016, there were 25,000, while in 2018, we went down to 15,305 deaths.
The number of infections went down as well. But the fight is far from being won, with many victims, including among youth, or those most vulnerable: MSM, trans, drug users and sex workers.
This situation is not a fatality. More investment will ensure curbing the epidemic. Experts estimate that 18 billion USD are necessary. Ivory Coast has understood that more funding is needed to strengthen healthcare, information on health, and collaboration with decentralised entities. We are however convinced that this is not enough. Advocacy was made towards the Global Fund since 2009 to maintain what has been done so far. Ivory Coast has submitted and obtained funding for HIV, TB and malaria for a global fund of 192 billion for a period of 3 years from 2018 to 2020 to reinforce Ivory Coast’s healthcare system.
Ivory Coast has estimated a co-funding of 15% of this funding, and we are committed to this. We thank the Global Fund for its support in the implementation of its funding, and for the funding of healthcare. From 15-19 April, we will have a national dialogue on funding with the support of all stakeholders. Therefore, Ivory Coast is honoured by the decision of the French government to hold the conference of the Global Fund in Lyon in October, in order to end HIV, TB and malaria by 2020, as planned in the SDGs.
The support of the Global Fund would not be adequate unless these efforts are sustained. In the name of those affected by these diseases, we need to continue the financial support of the Global Fund. We give our thanks to France for its ongoing support and work in this regard, as well as all those involved. Many thanks to all of you, healthcare providers, to guarantee an optimal health status.
Dr Nicolas Prisse, MILDECA, France. Thank you very much. I am very happy to be sharing these discussions today and to the Minister from Ivory Coast, we support the engagement of your government. HIV, TB and malaria remain priorities, in particular for those most at risk, including drug users who are at high risk, both for HIV and for hepatitis C. Support in healthcare, support and harm reduction without stigma, judgement to prevent harms is an essential component of a balanced approach towards addictive behaviours. If many countries have made harm reduction as a key pillar, it is because it is an effective measure. The consensus of the scientific community is clear on harm reduction and they invite us to develop and mobilise to reduce fears around harm reduction.
We plan powerful measures to reduce risks, but these should always be improved. We have opened two safe consumption rooms since 2016 and we will aim to continue to develop and strengthen these experimentations. These have gone through rigorous scrutiny. We will do an economic and social evaluation and will have the preliminary results at the end of 2019.
We also support the mobilisation from the international community on international health aspects. We reiterate the importance of the Global Fund as included in the UNGASS and SDGs, including SDG 3. France has given more than 4 million euros since the Global Fund’s creation. The next conference will be a key moment, and will take place for the first time in France, testimony of our renewed engagement. We will aim to collect funding for 2020-2022, this mobilisation is fundamental to tackle HIV, TB and malaria.
I am happy we can go ahead as a common front, including civil society, which is essential for the coherence of our actions and our effectiveness. I would like to highlight the role of civil society. Community workers, families and patients have been critical in responding to the HIV epidemic. Sometimes we are not in agreement, but we work well together. They alert us of certain phenomena, help us go faster and better to help those most at risk, facilitate access to the human right of health. This will remain a French priority.
Kate Thomson, Global Fund to Fight AIDS, Malayria and Tuberculosis. Thanks to the governments of Ivory Coast, France and the French civil society platform. Millions of lives have been saved through the Global Fund, millions are currently under ART, treated for TB, and millions of nets have been distributed to prevent malaria. The government of Ivory Coast, civil society and the private sector have been key. Our efforts would not have been possible without this diverse partnership. We will have a replenishment in Lyon in October.
I probably don’t need to reiterate the need for harm reduction and its effectiveness in curbing HIV. We are proud to be the main donor for harm reduction. We allocated 232 million dollars in the previous round, including investments towards capacity building, direct assistance. But the gap in funding remains significant and a major area of concern. We need to remove human rights and gender-related barriers that prevent access. We have worked towards removing those barriers in 20 countries. We fund 7 key interventions in line with technical guidance: reducing stigma and discrimination, providing healthcare, sensitising healthcare providers, monitoring and reviewing policies, and reducing discrimination against women, including women who use drugs who face greater challenges.
Over the next five years, we will continue addressing these barriers. Inputs have been collected in each of the 20 countries.
Diverse partnerships have been established, making sure that voices, knowledge and expertise of people who use drugs are heard and valued, aligned with the principle of ‘nothing about us without us’. We therefore work with networks of PWUD at national and international level. We work with WHO and UNAIDS to ensure that our programmes are aligned. UNDP also acts as a principle recipient for our grants. UNODC is an important partner. We value the work of the HIV team in particular, especially for women who use drugs and people in prison. UNODC provides important links with other institutions. One important mechanism is the Strategic Advisory Group, set up by UNODC itself, which provides a platform for UNODC, UN and civil society to highlight needs, support each other to move the agenda forward.
But so much more needs to be done to bring programmes to scale, ensure that PWUD can access ART, to develop low-threshold evidence-based treatment such as OST, and to address stigma and discrimination against PWUD including women and youth. We need to do more to ensure quality programme implementation. We face widespread misunderstanding of harm reduction, lack of political will, and the existence of policies and laws that impede harm reduction implementation – including criminalisation of PWUD. And there is lack of funding for harm reduction.
I was reading the new UNAIDS report released yesterday. This highlights the scale of our collective challenge, and the need to address the health challenges and costs of repressive drug policies – as were highlighted by IDPC, Global Commission on Drug Policy and others.
The right to health is not just an absence of a disease but also the highest state of health and well being. I thank you all and call on you to support the Global Fund to continue to fund the harm reduction response, putting people at the centre of our responses, including PWUD.
Camille Spire, French civil society platform on drug policy. I’m going to speak in French now, to balance both languages used in this side event. I will take the floor in the name of civil society, in English! The French civil society platform on international drug policy exists since 2014, gathering 11 NGOs working on drug policy issues: AIDES, ASUD, FAAAT, Federation Addiction, MDM, NORML, SAFE, SOS Hepatites, IDPC. Our organisation represents a broad range of service providers around the country, advocacy, research and international programmes. For instance, MDM works in Ivory Coast on harm reduction, and Federation Addiction currently chairs the CSFD.
The dialogue between CSOs and the French government has been intense and very active throughout the UNGASS, but also post-UNGASS and in preparation to this Ministerial Segment. To speak of the Global Fund, it is now the main financial tool for harm reduction services. It funds more than 40% of all harm reduction services in low and middle income countries. There are millions of people living with HIV worldwide and 2/3 living in Africa.
There is a decrease in HIV related deaths, highlighting the successes in the fight against HIV, but 41% of PLHIV don’t have access to ART. PWUD accounted for 9% of new HIV infections. This is much higher in Eastern Europe and MENA. If we take the example of TB, ¼ of the world population has latent TB. 1.6 million died in 2017 of TB, which is a curable disease. We have a long way to go.
According to Harm Reduction International, the funding gap for harm reduction in low and middle countries is close to 90%. We have a long margin for improvement. Right now we focus on activity indicators rather than outcomes, and lack of essential interventions funding for activities like community mobilisation and advocacy.
There is also the issue of state accountability on domestic resources. When the Global Fund withdraws from countries, governments don’t take over and harm reduction shuts down. We have some examples in Eastern Europe and Central Asia. The Global Fund in transitioning states should enter in dialogue with governments and with people who use drugs. But there is also still a need for funding increases, for harm reduction in particular. This should be a key issue discussed at the replenishment conference. We are on track to achieve the 90/90/90 targets, but we have to increase the funding.
Recently, the Global Fund released its investment case in financial targets. To get to these targets, donor countries must increase their contributions. We also need domestic responses. We urge all governments to implement evidence-based policies, urge new donors to increase contributions to the Global Fund.
Olga Szubert, Harm Reduction International. Thanks to the French and Ivory Coast government and to the French civil society platform. My team provides strategic analysis on funding for harm reduction. My presentation will highlight the funding crisis for harm reduction in low and middle income countries. We cannot be serious about ending AIDS if we do not adequately fund harm reduction.
‘PWUD have been the biggest casualties of the global war on drugs’, this is coming from the latest UNAIDS report published yesterday to coincide with the Ministerial Segment. This is due to discrimination, criminalisation, stigma. There is a clear solution to this problem, it is called harm reduction – says UNAIDS.
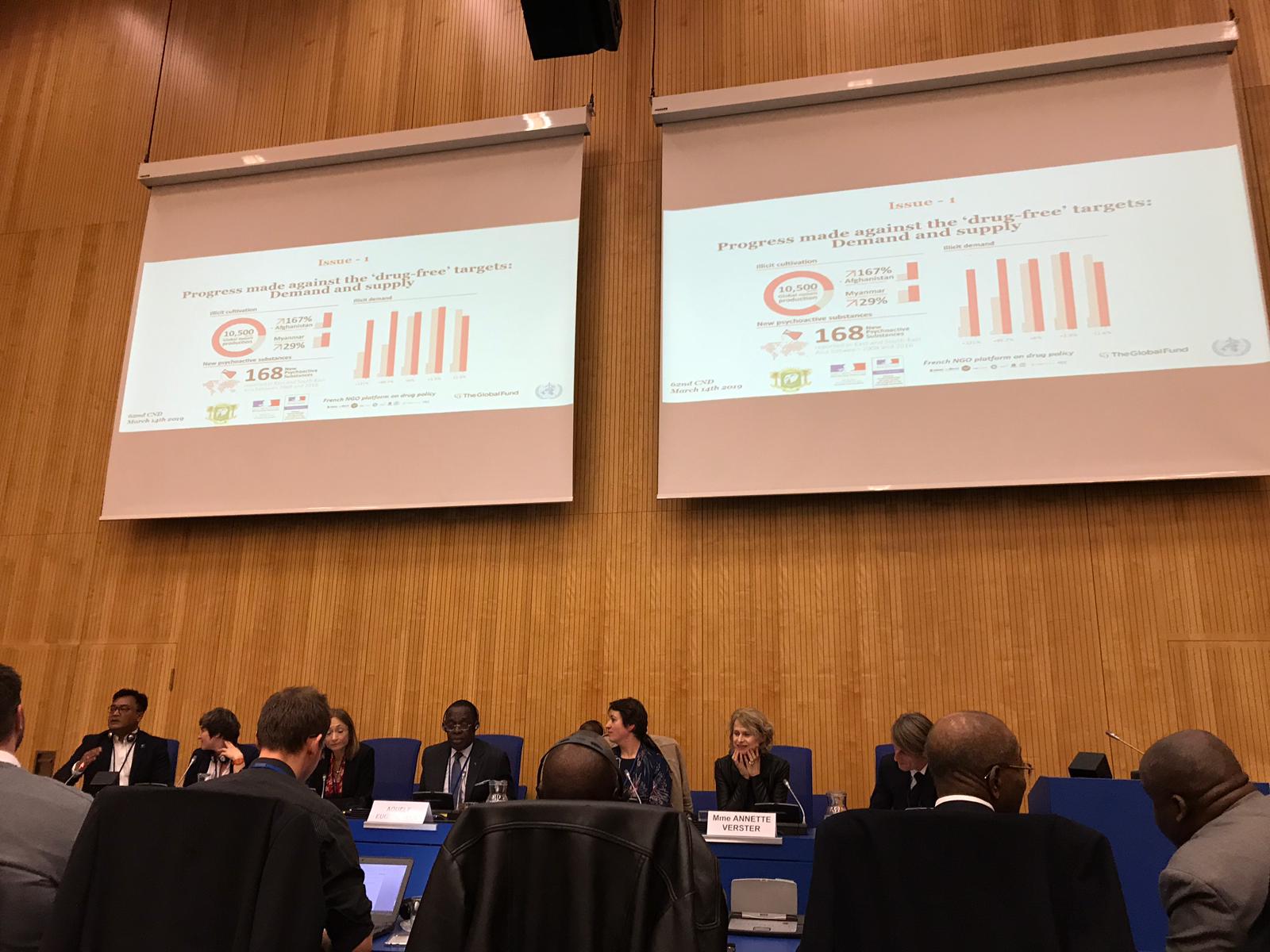
Every two years, HRI publishes its Global State of Harm Reduction. We started to map the responses since 2008. Since then we saw a steady increase in harm reduction, but it has then started stagnating. In 2016m, we had 90 countries using NSPs and 80 providing OST. In 2018, we had 86 countries providing NSPs and 86 OST. But there is a major issue of coverage, with the Lancet study concluding that 99% of people live in countries where coverage is too low.
Only 188 million is allocated to harm reduction (2016), while 1.5 billion would be required to prevent HIV among PWID so this is just 13% of what’s needed in low and middle income countries. There has been no increase in funding since 2007. Just 1% of donor and government spending went to HIV in 2016, and only 4 cents a day are spent per PWID. 64% of all funding for harm reduction still comes from international decades, and this is ¼ less than it was ten years ago. National governments are not stepping in to scale up funding for harm reduction.
Funding for harm reduction is in crisis. PWID are amongst the most vulnerable and HIV epidemics are commonplace in EECA and Asia. Harm reduction is integral to the HIV response.
Our key recommendations include the fact that international donors should invest in multilateral funding mechanisms such as the Global Fund – which is the largest donor, so if it is not as strongly replenished, we won’t have a strong harm reduction response. However, in parallel, the Global Fund should safeguard funding for harm reduction among PWID. International donors should increase harm reduction funding in line with epidemiological needs. Drug policy spending should be tracked and redirected to the most effective measures, including harm reduction, as is promoted by UNAIDS.
If achieved, we can end AIDS among PWUD by 2030 and achieve other goals on hepatitis C and overdose deaths. But without political will, this will not happen.
Charanjit Sharma, India HIV/AIDS Alliance. It is very fortunate, or by coincidence that I have been given the title of technical advisor on HIV and harm reduction in my organisation. I have been involved in drugs and harm reduction since 1986 as somebody who needed help and support. A lot of investment has happened, with modules, guidelines, strategies, examples of what worked. But the missing link is when a person uses drugs and needs help, and they cannot accept it. If you talk to any of the drug users like myself, we didn’t start using drugs so that by the age of 45 we would be dependent. I started just for fun, but I couldn’t find help when I needed it, and so I went on. But I learned through my life experience to use drugs safely. But people should have access to services. I am here talking to you because I had the opportunity to access buprenorphine, for the past 15 years. This is the reason why I am here speaking to you today and speak on behalf of my community. There were serious incidents where I could have lost my life had I not accessed naloxone when I suffered from an overdose. These are just some things I wanted to highlight here before going into my presentation.
We have many good things in front of us, because many people are coming together to understand what is drug use, what good or bad projects can be, what has been implemented successfully. Having said that, we still have problems. The number of countries reporting injecting drug use has increased, and will keep on increasing. The number of HIV and hepatitis C infections, overdose deaths and incarceration are increasing. On the other side, there are good programmes, but these are not enough, we need to do more if we want a successful harm reduction programme accessible to all who need them in all countries.
I will leave this slide to the audience – are we going in the right direction or is there something that we should do differently? I won’t go into detail here, but the numbers show that the numbers are increasing everywhere in terms of production and use. Production is not just happening in Myanmar, but in Afghanistan and other countries in Asia as well. Whatever technology used to prevent the production of drugs won’t work because people will find a way to continue the drug business. Many of the speakers have also talked about the right to health, the impacts on HIV, hepatitis C and overdoses. People can be arrested for drug use, but also for possessing clean needles and syringes – so people will not come to our centres because of barriers created by law enforcement and other groups working on demand or supply reduction.
This next slide is interesting: if you invest 1 dollar for harm reduction, the return is almost 6 dollars. If you invest 1 dollar for incarceration and detention, the return is very low in terms of public safety gains.
I want to present three principles here: listen to the drug user (they will provide you with what the issues are, understanding on programme design), listen to the drug user (what can be done and improved), and listen to the drug user (Support. Don’t Punish: protect the right of people who use drugs).
I want to add one more thing: 90/90/90: I want to translate this more into harm reduction: 90% of PWUD should have access to clean equipment, of that 90% of injections should happen safely without loss of life or overdose, and of that 90% of those should not have their rights violated, not be stigmatised or discriminated against, including women who use drugs. Programmes should be designed by women who need those programmes. The needs of men and women are totally different. In my country, we have several programmes, but they were designed by men, so women don’t come. We need to do things differently.
Camille. Thank you so much for creating this new 90/90/90 for us.
Annette Verster, WHO. Thank you all for organising this event and inviting WHO to speak and say something a word about interagency cooperation and commitments made in the UNGASS and the SDGs. The UNGASS outcome document gives a more prominent place to health and human rights, recommending a strong collaboration between agencies and partners. Recently, our collaboration with UNODC, INCB and others has been strengthened. WHO is committed and engaged in the implementation of UNGASS recommendations to advance the SDGs, especially SDG 3 on good health and well-being. Several health targets are particularly relevant, including SDG 3.5, 3.3. I want to also mention target 3.B on access to controlled medicines and 3.8 on universal health coverage.
WHO works with partners to achieve these targets. On target 3.B, as part of a balanced drug policy, we have adopted several WHA resolutions. 75% of the world’s population lacks adequate access to palliative care. WHO works with INCB and UNODC to conduct trainings.
On target 3.3, we are all aware of UNAIDS and its co-sponsors. UNODC is the convening agencies for harm reduction, with the strengthening of collaboration between UNODC and WHO through an MoU. Together with UNAIDS, we have collaborated at all levels: global, regional and in country to advocate and scale up harm reduction. We provide norms and standards, as well as technical support for programme implementation.
WHO has a strategic implementation framework with the Global Fund to ensure good public health strategies and ensure that nobody is left behind. Global Fund’s investments are consistent with our guidelines, including harm reduction for PWUD. We also collaborate with the Global Fund secretariat to implement the HIV package of interventions. We also convened peer review workshops to support new funding applications to the Global Fund, to ensure that applications on harm reduction are well articulated. We also support harm reduction implementation in countries like South Africa, Nigeria and Mozambique.
The Global Fund is the main donor on harm reduction. We provide technical expertise at global level and support Global Fund activities in countries.
Another key collaborative mechanism is the Strategic Advisory Group convened by UNODC, Norway, the Global Fund and UN partners. This group has advised agencies and donors on harm reduction over the past 5 years. We have focused also on the replenishment of the Global Fund, and met with the Executive Director of the Global Fund to discuss these matters, as a reduction in funding on harm reduction would have major impacts. WHO is undertaking unprecedented efforts to transform itself into a more effective and relevant organisation in the world we live in. Universal Health Coverage is key, and we want to ensure that harm reduction is included in the core health packages provided by governments.
Due to stigma and marginalisation, services for PWUD are often given low priority, and are often inaccessible, not affordable and of low quality. All the health needs of people, including those of PWUD are being met.
In summary, the WHO will continue to work on public health dimensions of the world drug problem. Collaboration with UNODC, INCB, UNAIDS, Global Fund and CSOs is critical in supporting the implementation of the UNGASS outcome document and in achieving the SDGs.
Questions and answers:
Celine Grillon, MDM. Thank you all for all the interesting presentations. It is important to bring these questions to the CND as health issues are very connected with drug policy. Could you provide thoughts on how to create stronger links between health and law enforcement agencies and to integrate harm reduction in different national drug policies.
Kate Thomson, Global Fund. I spoke a bit to our initiative to break down barriers in access, and I have been in a couple of country stakeholders meetings in Mozambique and South Africa. In terms of the barriers, we work with countries to bring all relevant partners to the table, this has included Ministers for Justice and a range of different actors and CSOs as well working in this fields. Having the space to talk in a pragmatic solution-focused way on how collectively these areas can be addressed has been a good model. Creating that space has been critical in finding solutions, although it is ambitious too. It is something we are trying and we are seeing some results.
Charles Some, REVS PLUS, Burkina Faso. I thank you for the quality of the exchanges. But there is a critical dimension which has not been discussed: on legislative questions. Even though we have harm reduction programmes, people who use drugs won’t participate in health and harm reduction programmes. Secondly, at the Global Fund level, what do we give in terms of guarantees to ensure that the needs of those communities most at risk are adequately considered.
Aouele Eugene Aka, Ministry of Health, Ivory Coast. You have raised an important question. Reforms are ongoing, but unfortunately it is taking time. Yesterday, I passed some text at the government council and in the cabinet to reform the health system. We need to reform texts that often date back to the colonial era. Last week, WHO met with us on how to harmonise all systems. We then met at the West African Organisation of Health, to discuss reforms. We must discuss of everything, and reforms are ongoing. We also need to regulate the pharmaceutical sector. I also wanted to add something: once we have reformed, we need to transform mentalities of all stakeholders, ensuring that health providers take the reforms on board. It is not just a financial problem. Health services should be humanised. Everything must be taken into account.
Kate Tomson, Global Fund. We can’t always wait for legislative reform in order to act. As the Minister said, reforms are ongoing and it’s long term. We need advocacy to push for reform, but it should not stop us to ensure that the right programmes are in place for the communities. The Global Fund has a framework to allocate funding to countries and those decide how to use funding. Important here is the need for civil society and advocates to be at the table and be a part of the conversation as decisions are made. An issue you have alluded to is that of data – it is hard to argue for programmes if the population is incredibly invisible. In terms of West Africa, it is a challenge for all of us but we are working together to address it together with governments and NGOs. I was meeting yesterday with our grant management head for West Africa and the need to ensure a greater focus on key population in programming for HIV.
Aouele Eugene Aka, Ministry of Health, Ivory Coast. Reforms must put the person at the centre. If it is not the case, they will not work. All stakeholders and people responsible discuss health coverage as a human right. Any reform not taking into account this key principle will fail. In Ivory Coast we are even talking about the social aspect, in particular for those most vulnerable.
Camille. Thank you all. The message is clear: funding, addressing barriers, ensuring access to services, ensuring more cooperation.