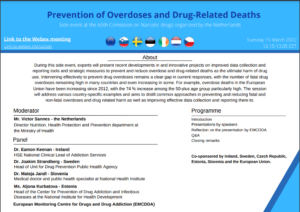
Organized by the Netherlands with the support of the Czech Republic, Estonia, Ireland, Slovenia, Sweden, and the European Union
During this side event, experts will present recent developments in and innovative projects on improved data collection and reporting tools and strategic measures to prevent and reduce overdose and drug-related deaths as the ultimate harm of drug use. Intervening effectively to prevent drug overdoses remains a clear gap in current responses, with the number of fatal drug overdoses remaining high in many countries and even increasing in some. For example, overdose deaths in the European Union have been increasing since 2012, with the 74% increase among the 50-plus age group particularly high. The session will address various country-specific examples and aims to distill common approaches in preventing and reducing fatal and non-fatal overdoses and drug-related harm as well as improving effective data collection and reporting there to.
Moderator: Mr Victor Sannes – the Netherlands, Director Nutrition, Health Protection and Prevention Department, Ministry of Health
Ms Aljona Kurbatova – Estonia, Head of the Center for Prevention of Drug Addiction and Infectious Diseases at the National Institute for Health Development
We were the number one country for drug related overdose deaths in the EU a few years ago. Lack of preparedness led to this escalation – services weren’t ready to address the synthetic opioid crisis. Our project aims to answer the question: how can countries be prepared to address this issue? How to evaluate whether you are prepared to address this issue. We are also preparing an evidence based toolkit – early warning systems, naloxone programs – what we need to tweak for synthetic opioids. We need experience and research-based solutions. Estonia is a tiny country in comparison to others. We are happy to publish the work that has been done to adjust drug checking services for synthetics – we will launch this in June – a lot of recommendations and tips to adjust your services. These substances are very dangerous.
Dr Eamon Keenan – Ireland, HSE National Clinical Lead of Addiction Services
We’re looking forward to St Patrick’s Day this week. Today we’ll talk about Ireland’s progress with naloxone in the past few years. Naloxone is prescription only in Ireland. Intranasal formulation is now available. We have a National Naloxone Quality Assurance Group.
70% of opioid poisonings are in men. We have seen a decline in deaths among people who use drugs since 2015. We looked at reported naloxone use – 569 reversals between 2018-2020. 75% of these were in Dublin, some were in Limerick. This is where we are planning to open the supervised injecting room when planning permissions come through. COVID-19 – we tried to get as many people into opioid agonist treatment as possible – this increased our capacity to also distribute naloxone.
One of the key responses we had was our engagement with people who use drugs – UISCE. In combination with this peer group, we co-designed resources on harm reduction and naloxone – we couldn’t have done it without them.
Our DOH calculated that our program saved 22 lives and saved approximately ~670 000 euro. We have received more funding for our naloxone program and we look forward to sharing the results of our successes in the future.
Dr Joakim Strandberg – Sweden, Head of Unit for Drug Prevention Public Health Agency
We are implementing a new early warning system for narcotic drugs in Sweden. We identified the need for a secure system – new registrations are monitored and moderated by our moderators. You can see the examples on the slides. There are 320 users in the system currently. Drug user organisations are also important members of the system. Its important that we moderate how the system disseminates information. We need to ensure the system shares the right type of information to people who use drugs and that they can share the information with others. We have done some surveys – that conclude that the system so far is very useful.
Dr Mateja Jandl, Slovenia – Medical Doctor and Public Health Specialist, National Health Institute
I will present a comprehensive approach to address drug related deaths in Slovenia, as the number of deaths is increasing. Deaths per million in Slovenia is 51, compared to an EU average of 14. We have four approaches to reducing opioid mortality – implementation of take-home naloxone and reducing vulnerability through a well developed network of NGOs working in harm reduction. Reducing the risk of overdose – providing accessible opiate substitution treatment. Integration of services – we provide a network of mobile units, substance analysis laboratory, comprehensive psychosocial and medical treatment, rehabilitation; and prevention of infections and overdoses. In the pandemic, our services became more integrated – and we now see how important this is in reducing overdose deaths in Slovenia. Slovenia is geographically well covered with harm reduction services – day centres, mobile units and substitution treatment programs, in every region of Slovenia. Sharing our best practices: early warning system (a good national and regional network), safely and effectively administering pain relief therapy, and take-home naloxone – this is a priority for Slovenia and has been introduced in 2021. We will expand the THN program in 2022.
Jane Mounteney, European Monitoring Centre for Drugs and Drug Addiction (EMCDDA)
The presentations today show the risk and varied experiences in Europe. I note the amount of innovation, and the timeliness of the presentation in relation to the drug market – increasing range of drugs causing overdoses. World events at the moment will affect these programs. A focus on drug treatment, harm reduction and preparedness is needed at the moment.
At the EMCDDA we work with a 3-tiered framework: the base is broad interventions that are about reducing vulnerability e.g. housing and stigma reduction schemes. Second level: focus on overdose, reducing overdose risk e.g. opiate substitution treatment, harm reduction services, early warning systems – but 4% of overdose result in death. This is the top level – overdose death prevention – take home naloxone and drug consumption rooms. There is a need for a systems approach, bringing in responses from all levels, and tailored to the country’s needs. Excellent work in cooperation and collaboration with people who use drugs for these services – this is very important. Evidence in this area for overdose prevention – there is strong evidence for opiate agonist therapy, take home naloxone programs. Emerging evidence and promising practice for other programs to try – evaluation is very important – to support this, we need to improve national data collection and reporting. Finally – we can share and learn from each other for best practices.
Anja Busse, UNODC
UNODC-WHO SOS Program – introduced at CND in 2017 with take home naloxone in four countries – Kazakhstan, Kyrgyzstan, Tajikistan, and Ukraine
14000 likely to witness an overdose have been trained and provided with take home naloxone. 90% of participants reported using naloxone when witnessing overdose, and in almost all instances the person was reported to survive (at least 400 lives were saved in less than 9 months). We would be happy to support other countries in this regard. Please join the community empowerment side event in 10 minutes to hear more on the SOS study.
Q&A:
Q: Scotland and Ireland – are there any collaborations? Yes, we are writing a paper together. There are problems with polydrug use in both countries. Aging population of people who inject drugs in Scotland. Scotland training police in take home naloxone. Important to get service user voice to the table.